Jan
26
HIDDEN IN PLAIN SIGHT
Filed Under Combat PTSD, Life, Peace, PTSD, TBI & PTSD, Tears of a Warrior, Trauma, War, Wisdom | Comments Off on HIDDEN IN PLAIN SIGHT
by Janet J. Seahorn, Ph.D

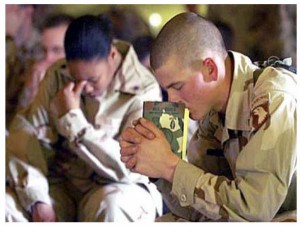
There is a phrase that one hears every now and then, Hidden in Plain Sight. Four simple words that eloquently reveal the complexity of the impact of trauma on one’s mind, heart, and soul. We see the person; we look at the eyes, the body language, the being’s form. The suffering is present in plain sight for all to witness. Yet, few do, lacking the keen observational heart skills required to notice anguish.
There are days I wish I didn’t see it – the faces of children battered by abuse and neglect; the adolescent’s depressive absorption into the ugly world of alcohol and drugs, and the veiled, but ever present ghosts of veterans, young and old carrying their memories of war. They haunt me as the world moves around their pain because it is hidden in plain sight.
Much like ‘Don’t Ask, Don’t Tell’, we are a nation that prefers to maintain our equilibrium at all cost. We tend to be uncomfortable with sorrow even when it stands knocking at our front door asking only for recognition and a bit of compassion.
We say we are a nation of empathy, yet often dismiss the humanity that exists in every person, especially those with whom we don’t agree. We argue we are intelligent, proficient thinkers, yet fight rigorously to disqualify any information that does not align with our personal paradigms/beliefs, whether true or misleading, without accurate evidence or data.
The answers to our current and future problems are available, but for too many they are hidden in plain sight. It will take incredible courage to look into our own minds and hearts searching for what is right and true. It will take courage and honest self-reflection to heal the hidden wounds of the wounded, but it can be done. What lies before us does not need to consume us with fear or apprehension. When confronted, trauma and pain can be overcome and no longer hidden or carried alone.
Light and sunshine are incredible healers.
Dec
31
SCOOBY DOO AND A NEW YEAR TOO
Filed Under Dogs, New Year, Peace, TBI & PTSD, Tears of a Warrior | Comments Off on SCOOBY DOO AND A NEW YEAR TOO
 by Janet J. Seahorn, Ph.D
by Janet J. Seahorn, Ph.D
Hard to believe it is the end of 2010. What an interesting year this has been. Most of our days have been filled with many blessings of meeting new friends, spending time with old ones and beloved family members, taking part in all of nature’s wonderful opportunities, and just having some time for personal rest and relaxation. To close out this year, I thought I would mention just a few of our many blessings.
While Tony was going through some medical tests at the Cheyenne Vet Hospital last week, I met a very large great Dane named Scooby Doo. He was a rescue dog who became a therapy companion for one of the wheelchair bound vets. While others believed this dog was vicious and untrainable (due to abuse from several prior families), the vet saw goodness and potential. Turns out that love does make a difference and Scooby Doo is living proof.
As stated, spending time with family and friends is always at the top of our list. There are never enough minutes in the year to let others know how much they mean to us. How their phone calls, get-togethers and small interactions are the best rewards of every day.
Being able to attend several veteran’s reunions and conventions humbled us greatly. Meeting with the Black Lions in Las Vegas, Nevada, showed us again the enormous sacrifice vets give. This particular group endured some of the worst combat missions in the Vietnam War, yet they continue to move forward every day with hope and courage. In August we were guest speakers at the annual Nebraska Vets Convention in Norfolk, NE. The veterans and their spouses were so gracious, we enjoyed the entire event.
In June Tony was the keynote speaker for Project Healing Waters’ annual organizational meeting. The conference was held in Steamboat Springs, CO, a truly stunning and perfect setting for an organization dedicated to introducing wounded vets to the beauty and peace of fly fishing. Often times, nature and our four-legged, long tongued companions are the best medicine for a tattered spirit and injured body.
For Memorial Day, we traveled to Evanston, WY to speak to a patriotic community and address the sacrifices made by all veterans from all generations.
The return home from Iraq of the Wyoming National Guard in March was a moment of jubilation that words can’t quite describe. Families who diligently carried on everyday duties without their loved ones were significantly relieved to finally have the tour of duty complete. Then in February, a group of citizens from Ft. Collins purchased and presented a beautiful Quilt of Valor to the Fort Collins Veterans Center. The quilt was made by Donna Roche in Rogers, Arkansas. Her group of quilters sends quilts overseas to various vet hospitals in the US as gifts of comfort and hope to wounded warriors.
We hope your list of items holds similar stories of warm get-togethers, memorable adventures, and quiet gratefulness. Thank you again for your many comments, your support, and most of all your immeasurable service to our country.
Jan and Tony
Oct
12
Dang – These Stats Are Amazing
Filed Under Black Lions, Combat PTSD, Life, PTSD, TBI & PTSD, Tears of a Warrior, War | Comments Off on Dang – These Stats Are Amazing
by Janet J. Seahorn, Ph.D.

As you might imagine, we have been doing research and accumulating multiple types of data for well over ten years. Much has been on PTSD along with statistics on various numbers of vets who served in different wars, as well as their injury and death counts.
Over the last two weeks we have had numerous individuals send us a variety of articles and information on the Vietnam War. Perhaps the most startling was a number that I checked out through several sites; it was a number that claimed only 1/3 of veterans who served in Vietnam are still alive. This number was part of a 2000 census count, so I can only assume the number is far lower ten years later. The actually statement was “Of the 2,709,918 Americans who served in Vietnam, less than 850,000 are estimated to be alive today”.
Yikes. This is a number neither Tony nor I ever expected. Perhaps we don’t want to admit that we are growing that much older. Or perhaps the numbers may show an underlying concern with the health of Vietnam vets who endured massive amounts of toxic chemicals while serving in the war zone. At any rate, the small number of Vietnam vets still living is a real worry.
Another statistic that we have seen is that of the 9,087,000 military personnel who served from August 5, 1964 – May 7, 1975, only 2,709,918 actually served in Vietnam. Of those who were in Vietnam, only around “40-50% either fought in combat, provided close support or were at least fairly regularly exposed to enemy attack” (Bob Beavis, 2010).
And most alarming in a 1995 census around 9.5 million individuals falsely claimed that they had served in Vietnam when they had not; in the 2000 census almost 14 million individuals falsely made such a claim. Yikes, no wonder the Veteran’s Administration is having a harder time trying to identify who did and did not serve when there are so many “false” claimants in America. As my grandmother would say, “Shame, shame, on all of them”.
Last, and this I find very interesting given the amount of press that has been given to the number of Vietnam vets who were supposedly alcoholics, drug users, and homeless, according to various vet sources (VFW Magazine, the Public Information Office…) there was/is no difference between those populations who served in Vietnam and those who did not.
Also, we often hear about how many Vietnam vets ended up in prison… simply not true. Vietnam vets were less likely to be in or served time in prison – only ½ of one percent (Bob Beavis). Over 82% of Vietnam veterans seemed to have made a pretty successful transition to civilian life in spite of dealing with severe injuries and PTSD.
So congratulations all you Vietnam vets; you have lived a truly exceptional life, served your country with honor, and had the incredible strength and internal courage to continue to live life with high principles and personal pride.
Jun
30
PTSD Series Discussion #5
Filed Under Brain Injury, Combat PTSD, PTSD, PTSD treatment, TBI & PTSD, Tears of a Warrior, Treating PTSD, War | Comments Off on PTSD Series Discussion #5
By Janet J. Seahorn
When is it time to seek outside help?
This is pretty easy to answer: You will know if it is time to seek outside help when the behavior of the serviceperson becomes abnormally un-normal. When life becomes a teeter-totter of ups and downs that can’t seem to be controlled no matter how hard you try. When your surroundings and relationships seem unstable and unsafe and you aren’t sure why, get help.
When my husband began experiencing PTSD, neither one of us had a clue what was going on at the time. There was no such thing as Post-Traumatic Stress. War was something that a person went to, came home from and tried to move on. It wasn’t discussed. It wasn’t thought about (or so we once thought and wanted to believe).
No one considered how the events of combat could impact an individual for the rest of his life. If you came home somewhat physically whole, that was a gift. You healed physically, and you lived as if all the horror from battle never happened. The past was the past and it should not impact one’s future. What an absurd assumption.
Now we understand that nothing in our past is ever fully in the past. The good and the difficult follow us wherever we go. We are part of our experiences. With understanding, courage, and information we may gain strength and wisdom to move forward. Getting outside help can guide us in forming the wisdom and understanding needed for healing.
What are some good resources for help with PTSD or TBI?
There are many resources available to our military service men and women. Check with your local Veteran’s Administration Center if you suspect you need support. You may need to be referred to a Veteran Hospital for further testing and diagnosis, especially if you suspect a traumatic brain injury. Every state has several local centers that have been established to help veterans find the appropriate placement and support needed to get the services they may require. (VA Centers are listed in our book)
Don’t stop at NO if you are convinced you have something wrong that necessitates some form of treatment. Sometimes all you need is that one special person who can take your situation seriously enough to get help. Our family personally saw this happen with my brother. He was extremely wary of anyone associated with the government. As a Vietnam vet, his mistrust of a broken, ineffective system made him reluctant to seek help from a military or veteran organization of any kind. Once he decided to seek services he ran into several brick walls. Yet, he kept trying, until he finally found a former army sergeant who took his situation seriously and made things happen.
It only took one person to make a difference. Don’t’ give up or give in to frustration. Keep going. Help is available, but sometimes you may have to fight for it just like you did in battle. If you did it then, you can do it now.
In ending, we want to thank you and your loved ones for your service and sacrifice. You have made a difference that few will understand, or perhaps fully appreciate. Nevertheless, please recognize the depth of your courage, strength and warrior spirit. These are the attributes that sustained you through combat, and now they will do so again in moving you towards healing and a better life.
May
13
PTSD Series Discussion #1
Filed Under Combat PTSD, PTSD, PTSD treatment, TBI & PTSD, Tears of a Warrior, Treating PTSD, War | Comments Off on PTSD Series Discussion #1
 Several weeks ago we were ask to respond to a set of questions regarding Post-Traumatic Stress and combat vets. These responses will be used in a short pamphlet/flip book that will be distributed through another organization. We thought many of our readers might find the questions and our feedback useful. Today’s blog is the first of our five part series. (Part 1 of 5)
Several weeks ago we were ask to respond to a set of questions regarding Post-Traumatic Stress and combat vets. These responses will be used in a short pamphlet/flip book that will be distributed through another organization. We thought many of our readers might find the questions and our feedback useful. Today’s blog is the first of our five part series. (Part 1 of 5)
•1. How do I know if my serviceperson might be suffering from PTSD? (Symptoms, possibly)
This is a great question with a not so simple answer. Not every person who returns from serving in a war zone ends up with Post-Traumatic Stress. A great deal depends on the amount of time the person spent serving under combat conditions, as well as how many traumatic events occurred during his/her deployment. Most doctors and researchers agree that the more time spent away form home, and the more distressing events experienced during each deployment, the greater the likelihood the person may experience some form of PTSD. If the individual was already predisposed to stressful home or environmental factors before joining the military, PTSD may become even more prevalent. There is no simple formula for why one person develops PTSD while others seem OK. But one thing is certain; it has nothing to do with a lack of strength, courage, or character. Sometimes it is simply the hazard of war due to exposure to unspeakable traumatic events, often in life and death situations.
So what signs might you look for when suspecting someone has PTSD? Since the brain is restructured by every act it experiences, it is sensitive to many good and not so good events. Love, hate, prejudice, kindness, and violence are just a few life experiences. Yet, when the life-threatening events occur over and over again for a long duration of time, or even during one incredibly horrifying event, the mind/brain is seared with the image and emotional feelings become imprinted.
Signs/Characteristics of PTSD:
- ð Hyperarousal and abnormal startle responses
- ð Irritability and/or jumpiness; constantly on guard
- ð Hypervigilance
- ð Nightmares, insomnia, and night sweats
- ð Recurrent traumatic memories or flashbacks
- ð Overwhelming waves of emotions
- ð Survivor guilt
- ð Feeling detached and/or emotionally withdrawn from others
- ð Fragmented sense of self and identity
- ð Panic attacks
- ð Shame
- ð Despair
- ð Lethargic or lack of motivation/interest in life, work, and family
- ð Avoidance of common places, activities
- ð Memory and concentration problems
- ð Sadness and hopelessness about the future
The key here is that a person generally does not have ALL of these symptoms at once. Some come more often than others. One person may have numerous panic attacks, while another may want to isolate himself and not take part in normal daily and family activities. It is the severity and frequency of the symptoms that would suggest a diagnosis of Post-Traumatic Stress.
Oct
13
Brain Trauma, Soul Trauma
Filed Under Brain Injury, TBI & PTSD, Trauma | Comments Off on Brain Trauma, Soul Trauma
by Janet J. Seahorn
 OK, here is something to ponder; can Brain Trauma cause Soul Trauma?
OK, here is something to ponder; can Brain Trauma cause Soul Trauma?
By “brain trauma”, I mean a traumatic brain injury, a verifiable medical condition caused by some insult to the brain, i.e., car accident, falling, hitting one’s head, being in or close to an IED explosion, shaken baby syndrome, stroke… and the list goes on.
Every year over 1.5 million Americans experience some type of traumatic brain injury (TBI).
Personally, I believe the number is higher, as many incidents never get reported because no one knows or realizes that such a trauma has occurred. Which is why all of the information on TBI makes me muse over what actually goes on in the brain/mind, body, and soul when it has been injured?
I think about the mind and wonder how such a magnificent organ can be in command of so much in a person: body, emotions, perceptions…
I think about the soul and wonder how such an invisible concept can make such a difference in one’s life; a difference that gives one strength, courage, and hope to make it through some truly desperate times.
I think about how anyone who experiences a restructuring of the brain after some internal or external trauma can move forward in ways that are nothing short of miraculous. A healing that leaves the brain changed, but the person still functioning.
I think about how the soul and spirit must somehow be part of the healing that takes place in the organ called the brain. How the soul/spirit may give some kind of divine direction to the mind that allows it to mend. In many cases it may not mend itself back to its original state but reorganizes in such a manner that perhaps enhances the individual with greater compassion, humility, and fearlessness.
I’d like to believe that angels watch over us and it is this entity that connects the mind, soul, and heart. Noah benShea thoughtfully noted, “Faith sees around corners”. Maybe these celestial beings are also within the corners of our battered minds, soothing, comforting, and mending.
Most days, though, I am just immensely appreciative that something more powerful than I can ever imagine is taking some charge over all of our well-being, perhaps from that place we call Heaven.
Jul
29
Comparing TBI Injuries and PTSD
Filed Under TBI & PTSD | Comments Off on Comparing TBI Injuries and PTSD
 Last blog we focused on Traumatic Brain Injuries and how similar they can be to the symptoms of Post-traumatic Brain Disorders. To help demonstrate these similarities I have created a chart of Similarities and Differences.
Last blog we focused on Traumatic Brain Injuries and how similar they can be to the symptoms of Post-traumatic Brain Disorders. To help demonstrate these similarities I have created a chart of Similarities and Differences.
Much of the information is taken from our book, “Tears of a Warrior: A Family’s Story of Combat and Living with PTSD” and soon to be released new book by Laura Whittemore and Mary Ann Keatley, PhD, CCC, “Recovering from Mild Traumatic Brain Injury (MTBI): A Handbook of Hope for Our Military Warriors and Their Families”.
The Whittemore/Keatley book will give some helpful information on MTBIs including numerous questionnaires to assist individuals in recognizing if they need to seek medical services.
Note: Differences will be highlighted in Yellow (MTBIs) and Green (PTSD)
|
Mild Traumatic Brain Injury (MTBI) |
Post-traumatic Stress Disorder (PTSD)
|
|
Physical Symptoms · Headaches · Loss of balance · Vision problems · Dizziness · Loss of sex drive · Loss of energy · Easily fatigued · Sensitivity to light, sound, touch · Sleep disturbances |
Physical Symptoms · Headaches · Loss of sex drive · Loss of energy · Easily fatigued · Sleep disturbances · High blood pressure · Difficulty with digestion · Lower immune systems · High or lower levels of cortisol |
|
Emotional Symptoms · Depression · Mood swings, outbursts · Fearfulness · Apathy · Low motivation · Gullibility · Feeling easily overloaded · Anxiety, frustration · Difficulty managing emotions · Hyper vigilance, exaggerated startle response · Sense of helplessness · Loss of sense of self, low self-esteem · Nightmares · Anger |
Emotional Symptoms · Depression · Mood swings, outbursts · Fearfulness · Apathy · Low motivation · Feeling easily overloaded · Anxiety, frustration · Difficulty managing emotions · Hyper vigilance, exaggerated startle response · Sense of helplessness · Loss of sense of self, low self-esteem · Nightmares · Anger · Panic Attacks |
|
Cognitive Symptoms · Memory loss · Short attention span · Slowed thinking · Disorientation · Brain fatigue · Forgetfulness · Difficulty driving due to brain injury · Word finding and spelling difficulties · Impaired comprehension · Inability to organize thoughts · Inability to multitask · Inability to inhibit certain behaviors (i.e., excessive shopping, gambling…) · Difficulty with abstract thinking |
Cognitive Symptoms · Memory loss · Short attention span · Slowed thinking · Disorientation · Brain fatigue · Forgetfulness · Difficulty driving due to combat trauma… · Word finding and spelling difficulties · Impaired comprehension · Inability to organize thoughts · Inability to multitask · Inability to inhibit certain behaviors (i.e., excessive drinking, use of drugs both prescribed & illegal) · Difficulty with abstract thinking |
As you can readily see when you review the chart, the similarities are numerous which is why getting the most accurate diagnosis is critical. Treatment will differ by therapy options as well as prescribed medications. Improper identification can result in serious setbacks which may compound the individual’s ability to heal and recover from his/her injuries.
Jul
21
Traumatic Brain Injuries and PTSD
Filed Under TBI & PTSD | Comments Off on Traumatic Brain Injuries and PTSD
 It weighs barely three pounds, but it impacts everything that we do and much of who and what we are in life. The brain is a remarkable and sensitive body organ.
It weighs barely three pounds, but it impacts everything that we do and much of who and what we are in life. The brain is a remarkable and sensitive body organ.
This small, jelly-like form is made up of billions of neurons and their electrical/chemical connections that impact our emotions, our ability to remember new things, movement, and our interpretations of information from all the body senses (sight, sound, touch, taste…). When our brain is functioning well, we are able to do amazing things. Think about carrying out even the smallest tasks such as breathing, eating, watching a movie, or simply listening to music. The brain filters out unnecessary stimulus, thereby permitting us to transmit these basic, unconscious acts without much, if any effort. However, if we experience trauma to the brain, the entire system can be impacted in ways even the most knowledgeable neuroscientist doesn’t fully understand.
Now the simple tasks become much more complicated. The brain may not be able to filter out some things that allow us to focus on what is heard or seen. Or it may no longer be capable at breathing easily, or seeing accurately due to problems with concentration.
The notable piece of information to be aware of is the injury can be so cleverly disguised inside the brain that it can be difficult to diagnosis. A person does not have to pass out or get a knock on the noggin to acquire a brain injury. A huge blast, like those from an IED (improvised, explosive device), an unexpected fall, or rear-end car accident can jiggle the brain back and forth inside the skull causing internal bleeding and swelling. If and when this occurs, the normal functioning organ is no longer capable of doing what it once did so effortlessly. There is no such thing as a “perfect” brain. However, there is such a thing as a brain which has been damage.
Now, here’s the kicker in all of these particulars regarding the brain – the symptoms of Post-traumatic Stress Disorder and Mild Traumatic Brain injuries are very similar making identification of either problem tricky. Many individuals who have been involved in combat situations may have both PTSD and TBI to contend with as they cross the threshold to civilian life.
Therefore, it is critical that people who have either/both problems get medical services as soon as possible. The sooner the situation is attended to the better the results. Waiting only compounds the problem(s). If you suspect you have a problem, see a medical specialist and ask for a SPECT or an fMRI scan. SPECT scans must use machines that are at least a three – preferably four – angle apparatus. These give clearer pictures of the brain and what is happening when a person is doing particular tasks such as reading, thinking, or doing some specific task. CAT scans and regular MRIs don’t always pick up a slow bleed in the brain which is why SPECTS or fMRIs are needed for an accurate diagnosis.
Next blog, we will give some of the physical, emotional, and cognitive symptoms of TBIs and PTSD.

